In a career spanning four decades, physician Andrew Weil has gone from the sixties counterculture to the mainstream world of best-selling books and television appearances. Along the way he’s refused to compromise his essential view on medicine: that natural cures, lifestyle changes, and our own minds can match and even surpass the medical results of modern science.
Weil was born in Philadelphia in 1942 and had a childhood fascination with plants and herbal remedies. He received a bachelor’s degree in biology from Harvard University in 1964 and went on to get a medical degree there, despite his misgivings about the profession and what he perceived to be its limited approach to healing. He was nearly alone then in theorizing that whole plants, having coevolved with humans over millenniums, are more effective at treating illness than isolated or synthetic compounds.
During his time at Harvard, Weil began researching mind-altering substances found in nature. As an undergraduate he encountered Timothy Leary and Richard Alpert (now Ram Dass), who were studying the effects of LSD through the Harvard Psilocybin Project. Weil wrote his undergraduate thesis on the narcotic properties of nutmeg, and the journal Science published the results of his clinical study of marijuana while he was still in medical school.
After graduation Weil spent time at Mount Zion Hospital in San Francisco and at the National Institute of Mental Health before embarking on three years of travel in North and South America and Africa, where he studied traditional indigenous medicine. His experiences using psychedelics with shamans confirmed for him the importance of the mind in determining our health and even shaping our reality. In his first book, The Natural Mind (Mariner), Weil makes a case for the beneficial properties of hallucinogens and other drugs that he says expand consciousness and open new pathways in the brain.
In 1983 Weil published a comprehensive account of his views on medicine. Health and Healing (Mariner) proposes an approach that blends plant-based remedies and mind-body techniques with modern scientific methods. The book became a bestseller, and that same year Weil joined the faculty at the University of Arizona College of Medicine. In 1994 he established the Program in Integrative Medicine at the university — the first of its kind — with a goal to explore preventive practices, natural diets, botanical cures, and the mind’s ability to promote wellness. In 2008 the program became the Arizona Center for Integrative Medicine, of which Weil is the program director. Today there are more than forty similar programs at medical centers around the country, including the Mayo Clinic, Duke University, and Weil’s alma mater, Harvard Medical School.
Once a traveler on the outskirts of respectability, Weil has gained acceptance from many of his colleagues despite his continued critique of the medical establishment. He’s also found a large popular audience through his books, which include Natural Health, Natural Medicine: The Complete Guide to Wellness and Self-Care for Optimum Health (Mariner), Healthy Aging: A Lifelong Guide to Your Well-Being (Anchor), and Why Our Health Matters: A Vision of Medicine That Can Transform Our Future (Hudson Street Press), and through his appearances on Larry King Live and The Oprah Winfrey Show. His latest venture is True Food Kitchen, a health-food restaurant he opened in Phoenix, Arizona, in 2008 with restaurateur Sam Fox. The menu is eclectic, regional, and based on Weil’s own dietary principles. A second location has since opened in California, and more are planned.
At the age of sixty-eight Weil continues to push for an overhaul of institutional medicine in the U.S. He wants to establish integrative-medicine programs in every medical residency in the country and claims the integrative approach could cut the nation’s bloated healthcare budget by promoting inexpensive preventive measures instead of expensive drastic interventions. Though many still find his ideas controversial, few would question his influence on the debate over health in the U.S.
Weil and I spoke a few months before President Obama signed the healthcare-reform bill into law. Weil was visiting my hometown of San Rafael, California, to deliver a keynote address at the twentieth annual Bioneers Conference. Though he was relaxed, his responses were deliberate and carefully worded. He tempered his outrage over our current medical system’s dysfunctions with hopes for a more practical nature-based approach to healthcare in the future.
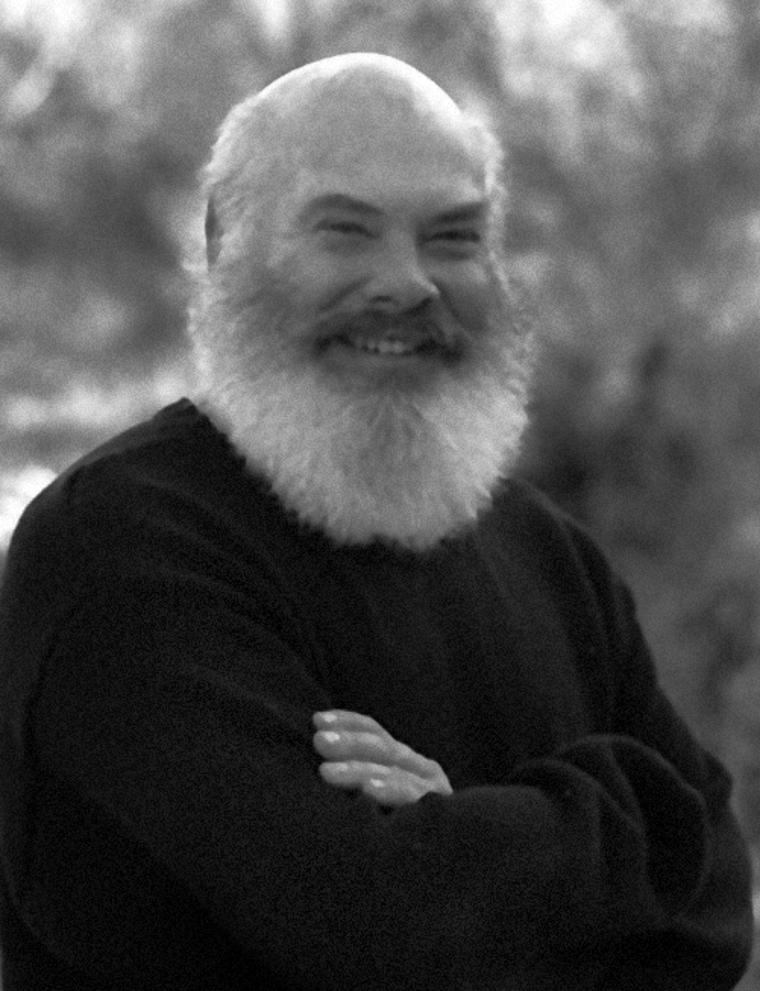
DR. ANDREW WEIL
Kupfer: How did you first come to appreciate the mind’s role in the healing process?
Weil: In the early 1970s I spent a lot of time in South America with native peoples, including shamans and healers. When Native Americans use the word medicine, it has a much bigger meaning than in our culture. Medicine men and shamans do not separate medicine, magic, and religion; it is all one. Their medicine has a capital M and includes a lot of what we would put under the category of superstition.
I had experiences with psychedelics and sweat lodges in both North and South America. These altered states of consciousness helped me see more clearly the limitations of treating only the physical body. Physiology is just one place to intervene. Good shamans are master psychotherapists, and I learned a lot from them.
Psychologist and philosopher William James said that normal consciousness is just one point on the spectrum of reality, and there are many, many others. I have found it possible to shift into these other states of consciousness and reality. I believe one may conceive of the world behind the veil without any detriment to one’s understanding of the world we know on this side of it. Bodies are important, but so are the mental and spiritual aspects of health. At the Arizona Center for Integrative Medicine our students — physicians, nurse practitioners, and medical residents — learn about meditation, sweat lodges, and other traditional medicine practices.
Doctors are the shamans of our technological culture. They have access to arcane knowledge and govern the province of life and death. But doctors are not trained to do the essential task of a shaman, which is to mediate between the invisible world and the visible world. How can you do that if you don’t believe there is an invisible world?
Kupfer: So you believe in a world we cannot see?
Weil: The Western scientific paradigm is materialistic, meaning that scientists do not believe in anything that cannot be perceived or measured. Look how restrictive that belief is. It’s the reason for the limited acceptance of mind-body medicine. The nonphysical causation of physical events is not allowed for in the reigning scientific paradigm. If you talk about nonphysical causes of changes in physical systems, materialists either ignore you or make fun of you or, if you keep at it, get angry with you.
Kupfer: But hasn’t interest in those topics increased in the decades since you were a medical student?
Weil: Yes, in the early 1970s I felt like a total loner. Now a lot of the ideas that fascinated me have become fairly mainstream. The change within the medical profession has been recent — I’d say since the early 1990s. It correlates with the economic deterioration of the healthcare system. As their financial situation has worsened, medical institutions have opened up to new ways of thinking.
Kupfer: Where do you see the nation’s healthcare system going?
Weil: Unless we transform it, it’s going to steer us into bankruptcy. At the moment the debate is mostly about health insurance, but that’s not the root problem. The root is cost, and I don’t think we can look to politicians to bring costs down. Both Republicans and Democrats are so beholden to the big-insurance and pharmaceutical lobbies that they are not free to act. If Congress can stop the big insurers from disqualifying people on the basis of preexisting conditions, that’s great, but these are little steps. Real change is going to come only if people get aroused enough to start a movement that shifts the balance of political power.
Also, if we don’t get serious about our health, it’s going to bankrupt us as a society. We already have the worst healthcare outcomes of all the developed nations, and we spend more on healthcare than anybody else. We’re spending something like 17 percent of the gross domestic product on it, and it could soon be 20 percent. That is simply not sustainable. And this is before the baby boomers reach old age and become the heaviest consumers of healthcare. We want universal healthcare, but we cannot extend our present disease-management system to all of our citizens. No one could pay all those bills.
Doctors are the shamans of our technological culture. They have access to arcane knowledge and govern the province of life and death. But doctors are not trained to do the essential task of a shaman, which is to mediate between the invisible world and the visible world. How can you do that if you don’t believe there is an invisible world?
Kupfer: Specialized medicine is the most expensive. How did we end up with so many specialists and so few generalists in American medicine?
Weil: The reason is obvious: specialists get paid more and have more prestige. But research has shown that countries and states with more primary-care providers have healthier citizens. To balance the system we could try forgiving student loans for people who go into primary care, but we need political organizing to promote these ideas.
Kupfer: Do you think there’s an opportunity now to get holistic practices covered by national health insurance?
Weil: Yes, but the priorities of insurance reimbursement are completely backward. We happily pay for interventions, diagnostic tests, and drugs, but we don’t pay for doctors to sit down and teach patients how to eat or how to relax. We talk about prevention, but that’s not where the money is going. One way to change those priorities is to conduct outcomes-and-effectiveness studies. Let’s look at five or ten common ailments that now cost us huge sums of money, such as type 2 diabetes or chronic back pain. Because conventional medicine has no magic-bullet treatment for these conditions, people often try complementary and alternative therapies. We could compare conventional treatment with integrative treatment (which might make selective use of conventional medicine) and assess medical outcomes and costs. I’m quite certain that integrative approaches would produce better results at lower costs. If we could get the data and show it to the people who pay for the nation’s healthcare, then they might change their reimbursement policies and start to pay for preventive and integrative medicine.
Kupfer: That will hardly be profitable to the corporate medical-industry establishment.
Weil: How do we make it profitable to practice prevention? I don’t know the answer to that. But it makes me very sad that healthcare is routinely referred to as an “industry” today. It never was in the past.
Kupfer: Do you believe a medical industry motivated by profit will ever act in patients’ best interests?
Weil: The interests and objectives of people who run for-profit healthcare institutions are fundamentally at odds with those of patients and doctors. One example is the overuse of expensive diagnostic scans. The people who own the equipment have to make their investment back, and they place enormous pressure on practitioners to order these tests, even when they’re not medically justified. Doctors should be able to make reasonable livings, and drug companies ought to be allowed to make fair profits, and maybe insurance companies, too, but not the outrageous profits that they are making now.
Kupfer: Is the medical orthodoxy starting to get worn down by alternative medicine?
Weil: Yes, but the orthodoxy is still focused on evidence-based medicine, which takes a scientific-reductionist view of healthcare. In practice, scientific reductionism has had damaging effects because it limits our ability to understand the natural world. It leads us to value isolated chemical compounds more than their complex sources in medicinal plants, which leads to overuse of powerful drugs that can cause harm. Evidence-based treatments are invariably pharmacological, because drugs are the only treatment the evidence-based community studies. In many places now you can’t present a lecture unless you submit in advance a summary to be approved by an evidence-based medical committee.
One of my colleagues in Norway, a research methodologist, is convinced that the way evidence-based medicine is practiced is a conspiracy of the pharmaceutical companies. It certainly works to their benefit, but the profit motive isn’t unique to drug companies. It pervades all aspects of American healthcare — orthodox, alternative, and otherwise.
Kupfer: What exactly is “integrative medicine”?
Weil: The general public thinks it’s the same as alternative and complementary medicine, but it isn’t. Alternative therapies are just one part of it. Integrative medicine first and foremost focuses on the body’s natural healing potential, which has been ignored in conventional medical education and training. To me the most wonderful feature of human biology is that our bodies can regulate themselves and repair and regenerate their components.
Integrative medicine looks at the whole person, because patients are more than physical bodies. To understand health and illness you’ve got to look at the mental and emotional and spiritual dimensions, not to mention the person’s involvement in a community. If you pay attention only to the physical body, you limit your interventions to those that are often the most expensive and the most potentially harmful.
Integrative medicine focuses on preventing disease and promoting health. Conventional medicine has failed us here, and that is one cause of the healthcare crisis. We are too occupied with managing cases of established diseases, most of which are lifestyle related and preventable. The essence of prevention is not colonoscopies and mammograms; it is understanding how our life choices reduce or increase the risk of disease. As a society we need to be helping people make better choices.
Integrative medicine emphasizes the doctor-patient relationship, which was once a major reward of practicing medicine. In the era of for-profit medicine, that relationship has been sabotaged. If you work in a corporate practice that requires you to spend only five to seven minutes with each patient, you can’t form the kinds of relationships that foster healing and provide emotional satisfaction. I think that’s a big reason many doctors are leaving the practice of clinical medicine. I know some who say that they would never let their child go into medicine today. Doctors are now as unhappy as patients.
Finally, integrative medicine embraces all therapeutic options that may be of value. That includes many that aren’t even on the radar of conventional medicine — simple, low-cost interventions like breath work and laughter therapy. The preference is for more-natural, less-invasive, less-expensive options whenever possible.
Kupfer: What inspired your interest in integrative medicine?
Weil: I came into the world very curious. A childhood interest in plants led me eventually to study botany, and then medical botany. I was also fascinated by the mind and how it affects the body. I tried to pursue those interests in medical school, but my studies were limited to standard fields. I was glad to get medical training, but I knew I didn’t want to practice the kind of medicine that I’d learned. So I began traveling to other cultures and learning about topics that I was interested in — mostly the relationship between what’s inside our head and what’s outside our head, and the possibility of changing external reality by changing internal reality.
Kupfer: Could you elaborate on the difference between plants and the powders distilled from them?
Weil: Because my early training was as a botanist, and because I had firsthand experience with medicinal plants, it was easy for me to see the differences between whole plants and molecules isolated from plants. But scientific reductionism declares the part to be equal to the whole. It is a convenient tool, as it makes it much easier to study the world, but it fails to capture the complexity of nature. Plants are master chemists that put human chemists to shame. Nature loves to invent molecules and elaborate on them exuberantly, trying out all sorts of variations. Typically medicinal plants contain families of related molecules. Often one molecule will account for most of the plant’s effects, like the morphine in opium, for example, or the cocaine in coca leaf. But the other molecules within the plant are variations on that main one, and within that complex mixture are what pharmacologists call “agonists and antagonists” — that is, molecules that push and those that pull, having opposite physiological effects. This accounts for the ambivalent action of some whole-plant drugs. There are plants used in Chinese medicine that are said to both lower high blood pressure and raise low blood pressure. That makes no sense to Western scientists. Our ideal drug is a magic bullet that has a specific effect. If drugs have multiple, especially paradoxical, effects, then we lose interest in them, because we think it means they don’t work by a specific biochemical mechanism.
Chinese medicine’s aim is to “dispel evil and support the good,” meaning the body’s natural defenses. In Western medicine we work only to dispel evil by fighting disease. Chinese philosophers classified drugs into three categories: superior, middle, and inferior. Inferior drugs are those that have specific effects in specific conditions, which is the ideal in Western medicine. A superior drug for traditional Chinese doctors is one that is good for everything, a panacea. They believe such drugs increase our bodies’ innate resistance.
Kupfer: What’s an example of such a drug?
Weil: Ginseng is a superior drug in the Chinese system. American ginseng, our native species, is highly valued in China. People in this part of the world took no interest in the plant for decades, except for the fact that people on the other side of the world would pay a lot of money for it. Starting in the early 1800s, some American-frontier settlers made their living harvesting ginseng almost to extinction to sell to the Chinese. Our scientists didn’t study it until the 1970s.
Ginseng is a wonderful “tonic,” a complex mixture of molecules that works smoothly with the mechanics of the body, both pushing and pulling. When you treat with plant remedies, you give the body a chance to participate in the therapeutic equation. Our highly purified pharmaceutical drugs give the body a strong shove in one direction, not allowing it any choice in the matter. That kind of treatment has its place. If someone has a life-threatening condition, you’ve got to get the body back in balance quickly. But for common diseases the natural preparations make much more sense.
Taking molecules out of plants is not the best way to work with nature. It is all part of the larger problem in American healthcare. We’ve got to start replacing either/or thinking with both/and thinking.
We are too occupied with managing cases of established diseases, most of which are lifestyle related and preventable. The essence of prevention is not colonoscopies and mammograms; it is understanding how our life choices reduce or increase the risk of disease.
Kupfer: How can the U.S. government raise the level of health literacy when agricultural, medical, and pharmaceutical interests exert such strong influence on policy in Washington?
Weil: We need the whole society to be united in this effort, meaning that the private sector, the government, and individuals all have to move in the same direction. At the moment that’s not the case. I’ve proposed that the Department of Education create an Office of Health Education to teach healthy life choices in elementary and high schools, drawing on innovative teaching methods like interactive video games that would help students see the real-world consequences of the decisions they make.
Of course, it’s hard to teach health and nutrition with a fast-food restaurant in the school cafeteria. Nor is it consistent to have the federal government telling us to eat more fruits and vegetables while the Department of Agriculture’s subsidies make junk foods the cheapest items in the grocery store and fruits and vegetables the most expensive. And we shouldn’t allow the big food manufacturers to make unhealthy foods attractive to kids through advertising. I just read that the American Academy of Family Physicians [AAFP] has formed a partnership with the Coca-Cola Company without consulting its membership. The AAFP will receive a grant to develop consumer education on beverages and sweeteners for a website of theirs. I can see the benefit to Coca-Cola, but what can the AAFP possibly gain except money?
Senator Tom Harkin of Iowa has worked to get subsidies for fresh fruits and vegetables and to make them available for free in school cafeterias. It hasn’t happened everywhere yet, but I hope it will. People eat what’s cheapest and most available, and what’s cheapest and most available right now is food that makes people fat and unhealthy. The spread of childhood obesity is creating an unprecedented epidemic of type 2 diabetes in the very young.
Kupfer: How about in medical education itself? Are you seeing some changes for the better in medical schools?
Weil: Only slight ones. The four years of medical school are so laden with information that it’s difficult to revamp the system. At the Arizona Center for Integrative Medicine we have been concentrating on residency training, because that’s where practice patterns are set and where change is possible. Our long-range goal is to get our curriculum adopted by all residencies in all specialties. Then we will have transformed medical education.
We also grant scholarships to physicians who pledge to provide care for underserved populations. Integrative medicine must not become medicine for only the affluent. But for that to happen, the priorities of insurance reimbursement must change.
Kupfer: Which countries have exemplary healthcare systems?
Weil: France is ranked number one by the World Health Organization, and Norway is also very good. No country does it completely right, however, and the problems that are taking our system down are growing in all developed countries. I would love to see medical doctors and other health professionals become more socially and politically active. They have been remarkably absent from the public debate.
Kupfer: What about Physicians for Social Responsibility?
Weil: That’s a good organization, but it’s not enough. The healthcare community needs to weigh in on the farm bill, for example, because the health implications of crop subsidies are enormous. Two years ago, when the farm bill was up for redrafting, an attempt was made to mobilize the healthcare community to influence the legislation, but it was ineffective. Mostly the medical profession has been absent from the process. Americans already consume more dairy products than they should, but when the dairy industry pressured the USDA to increase the number of recommended servings of milk products in the food pyramid, nobody from the medical profession objected. Doctors just abdicate responsibility in that area, as they do on the subject of environmental health hazards. If our government is given a choice between protecting public health and promoting private gain, it almost invariably sides with private interests. The medical profession, if it organized, could shift the balance of power.
Kupfer: Are other nations farther along in their adoption of integrative approaches?
Weil: Actually integrative medicine is far more established in the U.S., probably because our healthcare system is closest to collapse. Until the early 1990s I had a following in the general public, but I was not taken seriously by my medical colleagues. It was only when the economics of healthcare deteriorated that the University of Arizona supported my efforts to change medical education. Interest in integrative medicine is now being propelled by economic necessity.
As the crisis deepens, I think the wisdom of what we’re doing will become even more apparent. The big promise of integrative medicine is that it can bring low-cost treatments into the mainstream while preserving and even enhancing outcomes. I see nothing in the bills up before Congress that is going to lower the cost of healthcare. I’m disappointed that there has been so little emphasis from the White House on prevention and wellness. We have to get serious about prevention, and we have to end medicine’s dependence on expensive, high-tech solutions for every problem.
Kupfer: Do you include pharmaceuticals in the category of high-tech solutions?
Weil: Absolutely. The increase in drug consumption in our society alarms me. When I was a kid, Americans took drugs at about 10 percent the rate they do now. It’s easy to blame the drug companies, but they are just capitalizing on the mind-set that drugs are the only legitimate way of treating illness — and perhaps life’s problems in general. If you told the average doctor to manage a case without prescribing a drug, he or she would not know what to do. If a doctor doesn’t write a prescription, most patients will go looking for another practitioner. That has to be changed by educating both patients and physicians about the limitations and risks, as well as the benefits, of drugs. I would start by banning direct-to-consumer advertising of pharmaceuticals.
Some medicines are dangerously overprescribed: sleeping medications, antianxiety drugs, psychiatric drugs given to children, steroids, and stomach-acid-suppressive drugs immediately come to mind.
Kupfer: What Western medicines do you use?
Weil: I take a very low dose of Lipitor and two baby aspirins a day. I used to take red yeast rice to lower my cholesterol, but, given the history of heart disease on my father’s side, I wanted to get my LDL cholesterol lower, and Lipitor works well for me with no side effects.
Kupfer: Why is there such an aversion to natural solutions in the medical establishment today?
Weil: I had a conversation some years ago with the technical director of a German herbal manufacturer. He had lived all over the globe and told me he was struck by the extreme fear of nature in the English-speaking world. Germans, he said, have a long tradition of using natural remedies, and their government regulates herbal treatments the same way it does all medicines.
In our part of the world many people see nature as hostile, something to be controlled. Most articles in the scientific and popular media suggest that the products of laboratories are safe because they are known quantities, whereas the products of nature are wild and dangerous. I’ve seen many warnings about botanical remedies, but you can count on one hand the number of deaths attributed to herbal preparations in a year, and most of those are due to mistakes, where a product has been mislabeled, for example. The number of deaths caused by pharmaceuticals, by contrast, is enormous, even when they are used correctly. The word pharmacology comes from pharmakos, the Greek word for “poison.” There really is no difference between a drug and a poison except dose. Push the dose of any drug up high enough, and it becomes toxic. Bring the dose of some poisons down low enough, and they become useful medicines.
Kupfer: How do we escape the mind-set that drugs are the only way to treat illnesses?
Weil: The solution is education. Our center has graduated more than five hundred physicians and nurse practitioners who’ve received intensive, thousand-hour trainings. Our curriculum includes information about the body’s natural healing potential and alternative ways of managing illness.
Sometimes, however, education isn’t enough, and it takes direct experience to convince people. Many patients who come to us have had bad experiences with conventional medicine, including serious adverse reactions to prescription drugs. When they learn to deal with their conditions without drugs, they become grateful converts to integrative medicine. I’ve had many patients with chronic sinus conditions who’ve been on endless cycles of antibiotics and steroids. Some have had multiple sinus surgeries, with no benefit. I ask them to see what happens if they eliminate cow’s milk and everything made from cow’s milk from their diet for two months. A high percentage show dramatic improvement, sometimes complete remission. Then they ask: “Why didn’t a doctor tell me this before?” The answer is that doctors aren’t taught this.
Any effect you can produce in the human organism through a pharmacological intervention can also be produced, at least some of the time, purely by the mind. That is phenomenal. We should be investigating that mind mechanism with all our ability so that we can take greater advantage of it to treat disease and stimulate healing.
Kupfer: Could it be that people have come to believe so strongly in pharmaceuticals in part because of their past successes? It seems many critics of Western medicine overlook the miraculous developments of the past century.
Weil: Antibiotics, antihypertension drugs, and others can be very helpful if used appropriately, but most new pharmaceuticals really are not terrific. Many are worthless, and not a few are dangerous. If I were going to a desert island and could take only a few drugs, I would bring the old tried-and-true ones: morphine, aspirin, penicillin. For most products out there today, the manufacturers greatly exaggerate efficacy and downplay dangers, sometimes even actively concealing them.
The government should establish a compendium of objective information about drugs and require physicians to use it when they prescribe, instead of the industry publications they now use. The Physicians’ Desk Reference is put out by the pharmaceutical industry and is not objective. A medical-school pharmacology class gives better information — although that, too, can be heavily influenced by drug companies.
When I was growing up, if people had heartburn, they took Tums. Now heartburn is a medicalized condition called “GERD” — gastroesophageal reflux disease — and doctors put people on strong prescription drugs for it, drugs that block the production of stomach acid. These drugs were never intended for long-term use, because stomach acid is your major defense against infection through the mouth. So acid-blocking drugs increase your susceptibility to serious infections. They also increase the risk of stomach cancer and osteoporosis, and a recent article in the New England Journal of Medicine reported that if healthy people take these drugs and then stop suddenly, they develop GERD! So the drug can cause the condition that it is meant to cure.
Kupfer: That reminds me of how some antidepressants can actually lead to suicide.
Weil: I predict that many antidepressants, including Zoloft, Prozac, and Paxil, will be shown to work no better than placebos. The National Institutes of Health sponsored a much publicized study several years ago in which researchers tested Saint-John’s-wort against both placebo and Zoloft in depressed patients. Many newspapers reported the finding that Saint-John’s-wort worked no better than the placebo. What few reported was that Zoloft, too, also worked no better than the placebo.
By the way, I’m all for placebos. The fact that many people with mild to moderate depression respond to them is a good sign. To me the placebo effect is the meat of medicine: the patients heal themselves. That is the response you want to elicit. Instead of always trying to rule out placebo effects, we should be trying to encourage them. They are pure healing from within. Getting the maximum placebo response with the minimum intervention is the art of medicine, which is distinct from the science. But doctors are uncomfortable talking about placebos, because they think they involve deception. The word comes up most often in the question “How do you know that’s not just a placebo effect?” The key word here is just.
There is an assignment I have given to many medical students and doctors in our trainings: Pick up any publication of a randomized controlled trial of a drug and turn to the table summarizing the results. In the control (i.e., placebo) group you’ll always find a few subjects who showed all of the results produced in the experimental group, which received the drug being tested. To me this is the single most important finding of sixty years of randomized controlled drug testing. It means that any effect you can produce in the human organism through a pharmacological intervention can also be produced, at least some of the time, purely by the mind. That is phenomenal. We should be investigating that mind mechanism with all our ability so that we can take greater advantage of it to treat disease and stimulate healing. Let the brain centers and neurochemical pathways that control immune function and other physiological functions do the work.
Kupfer: But how does selling a placebo differ from selling snake oil?
Weil: I don’t think we should sell placebos. Rather we should try to take greater advantage of the placebo response by presenting all treatments with our full belief in them. When you present treatments to patients, your beliefs and expectations affect theirs, which affect the outcome.
Kupfer: You’ve said you are concerned about Americans’ use of sleep medications.
Weil: I am concerned about how poorly people sleep in our culture. The use of medications is at an all-time high, and these drugs do not reproduce natural sleep. Most of them suppress dreaming.
One detrimental influence on our sleep is our ability to light up the night, which is a significant change in our environment over the past hundred years. There’s a body of literature suggesting that exposure to light at night, even briefly, greatly increases cancer risk, especially risk of breast cancer in women. Women who are blind from birth have very low rates of breast cancer. Women who work night shifts have high rates of breast cancer. I tell people it is best to sleep in complete darkness, and if you have to get up in the middle of the night, don’t turn on the light, or else use a red Christmas-tree bulb, because it appears that light at the red end of the spectrum is safest.
Kupfer: What are your concerns about long-term exposure to cellular phones?
Weil: I have to qualify my answer: Like all doctors, I received no information about environmental health hazards in medical school. Zero. That’s an omission I’m trying to remedy. One of our center’s initiatives is the development of a curriculum in environmental health and medicine. Right now powerful vested interests influence what little information we do receive.
With cellphones there are certainly reasons to be concerned, and I’m a strong believer in the precautionary principle. We probably haven’t lived with cellphones long enough to know what their effects will be, but from what I do know, I advise people to limit usage and use hands-free devices. That is what I practice myself.
Kupfer: What are some healthcare myths that have been embraced by U.S. citizens?
Weil: The first is that we have the best healthcare in the world. That’s obviously not so. As I’ve said, our health outcomes are dismal compared to those of other developed countries. Medical care has grown increasingly sloppy in this country as a result of rushed visits and lack of nursing. Even in some of our best hospitals the care is iffy. You don’t want to go to a hospital unless you really have to. And we are seeing the outsourcing of surgical procedures to other countries, something that would have been unthinkable in the past. I know people who’ve had joint replacements in Belgium and Thailand and felt they got much better care than they would have received in the U.S.
Our medicine isn’t the best anymore. We depend far too much on drugs, our overuse of diagnostic procedures is risky, and we are not a healthy population. Some might believe that our medical technology puts us at a great advantage, but that technology has a shadow side. It is the main driver of healthcare-cost increases, and our infatuation with it diverts attention from the body’s intrinsic ability to heal and makes low-tech, low-cost solutions seem lackluster and old-fashioned.
Another myth is that we are ahead of everybody else in medical research. We do a lot of research, but the content is often irrelevant or off the mark. We don’t study treatments that could help us stay healthy or treat disease more cost-effectively. Also researchers are trained to think in limited ways. Most are interested in studying single-treatment interventions, whereas integrative medicine uses complex treatment approaches. We don’t just tell patients to take herbs; we also tell them to change their diets, use mind-body therapies, adjust their physical activity, and maybe try Chinese medicine along with a Western drug. Most researchers are uncomfortable with this sort of complexity. They want to know which component of an integrative treatment plan is responsible for what degree of benefit. We want to know how the whole plan works and how cost-effective it is compared to what conventional medicine recommends for the same condition.
The world is always teetering on the edge of disaster, but I believe that we can change external reality by changes in consciousness.
Kupfer: You consider yourself a medical conservative. How so?
Weil: Some people think that integrative medicine is radical, but I like to say it’s conservative, because we teach that the least treatment is the best: the least invasive, least expensive, and least harmful. If someone is critically ill, of course, you use drastic methods, but for ordinary ailments you want to let time and nature do the work of healing. We are fiscally conservative, because we are determined to lower healthcare costs by finding more-economical solutions. And we are philosophically conservative in that we’re trying to return medicine to its roots. Throughout history great medical philosophers have always recognized that healing is based in nature and the body’s capacity to heal itself.
Kupfer: People don’t feel they have a lot of time in our culture. How do you respond to someone who says that natural methods are too slow?
Weil: Maybe people have to find out for themselves that quick fixes are not long-term solutions and often have a much higher risk of harm.
Kupfer: How much of your job as a doctor is simply giving your patients your authoritative assurance that they can get better?
Weil: Many patients have told me, in retrospect, that the most important thing I did for them was to tell them they could get better; no other doctor had said that. I advise people not to stay in treatment with a doctor who doesn’t think they can get better. It’s too bad that so many doctors are pessimistic. It’s a consequence of training that’s skewed toward critical and advanced disease, where restoration of health is less likely.
Kupfer: What’s the function of the American Medical Association [AMA] in all of this?
Weil: [Laughs.] The AMA is largely irrelevant today. Only a minority of American doctors are members, so it isn’t representative of the profession anymore. Throughout its history it’s been ineffective as a lobbying organization. For example, chiropractors have gotten everything they’ve ever wanted: They got licensing in all fifty states. They got the right to use X-rays. They got the right to be reimbursed by insurance and Medicare. By contrast, the AMA has lost almost every battle it’s fought. It has also taken a strong stance against universal healthcare. I don’t think it counts for a lot these days.
Kupfer: You are the first and still one of the few people licensed to do medical-marijuana research in the U.S. How do you view the current debate?
Weil: It confounds me. After I did the first marijuana research study in 1968, I expected the plant would be legalized in ten years. I thought that if you got the information out there, people would change their minds. I quickly learned that was not the case. People’s beliefs about drugs are deeply rooted in cultural fears that are irrational and resistant to change. Nature-based remedies make many doctors and scientists uncomfortable, even though marijuana has lower toxicity than any other drug we know.
My early books The Natural Mind and From Chocolate to Morphine are about the root of our illegal-drug problem, which is our inability to come to grips with the human need for altered states of consciousness. It amazes me that we go on trying the same strategies to eliminate illegal drugs when the situation just gets worse and worse. But I see some willingness to abandon those strategies. Governor Arnold Schwarzenegger of California, due to economic concerns, has said that the approach we’ve been taking has not worked.
Kupfer: The U.S. government holds the patent on medical marijuana.
Weil: [Laughs.] If marijuana were legal and there were pharmaceutical versions of it available, the situation would be much better than what we have now. A practical problem for medical-marijuana proponents is that, for doctors to recommend it, there has to be a clear separation between recreational use and medical use. What’s going on in California looks an awful lot like recreational use. There’s a product in the UK called “Sativex,” a whole-marijuana extract in the form of an oral spray. It looks much more like a pharmaceutical product, and I could see doctors’ recommending it if it were available here. Most doctors I know are uncomfortable telling people to smoke marijuana or sending them to buyers’ clubs that look hedonistic.
Kupfer: Is there a patient of yours who best illustrates the power of self-healing?
Weil: A woman once came to me with severe eczema, so bad she’d been contemplating suicide. She’d seen the best doctors, and they’d put her on steroids, which hadn’t worked. I told her she could get better, but we would have to experiment. I suggested some dietary changes, some natural remedies, and hypnosis. She started using these methods, and the skin condition resolved itself over a few months. Her husband, a senior cardiothoracic surgeon, had been very skeptical about alternative therapies, but his wife’s success changed his mind. He took our fellowship in integrative medicine in his sixties and is now dedicated to advancing integrative methods.
Kupfer: You’ve gone from the cultural fringe to the mainstream. Have you in that process had to edit your message at all?
Weil: I don’t think so. I’m still controversial, which tells me I’m still doing what I’m supposed to do. It has been gratifying to watch the acceptance of my work, especially among the professionals who have been inspired by my writings and want to change how they practice.
Kupfer: For the most part you haven’t been attacked by industry watchdogs or conservative spokespeople. What’s your secret?
Weil: Maybe it’s because I don’t speak and write with an angry tone. People often have hostile reactions not to the content of what someone is saying but to the energy behind it.
Kupfer: You come across as very positive and optimistic.
Weil: I am optimistic. The world is always teetering on the edge of disaster, but I believe that we can change external reality by changes in consciousness. I continue to work toward that in myself and promote it to others.
Kupfer: Which of your teachers inspired you?
Weil: At Harvard I had the good fortune to be mentored by Richard Evans Schultes, who was the godfather of modern ethnobotany. I worked with him for a long time after I graduated. There was also an old osteopathic physician, Robert Fulford, who was the first person to make me aware of the natural healing potential of the human body. Other than that I’ve mostly followed my own intuition.
Kupfer: Do you have a spiritual practice?
Weil: Philosophically I’m most comfortable with Buddhism, but I’m interested in it as a practical philosophy, not a religion with ritual and dogma. I meditate; I try to connect with nature often; I strive to live in a nonharmful way and to follow Buddhist precepts about right living.
Kupfer: How have you experienced mind-body medicine in your own life?
Weil: I’ve written about the experience I had in 1971, when a lifelong cat allergy disappeared forever after I allowed myself to interact nondefensively with a cat during a blissful LSD trip. Critics have made fun of me for that, but it was the sort of powerful, positive experience that medical researchers should study.
One of my favorite verses of Laotzu is about how the empty space inside of a vessel is what makes it valuable. I believe in a world beyond our senses that impinges upon and shapes the material world. It is fluid and moldable. In some way consciousness modifies reality, and what we experience as external reality is a collective manifestation of what’s in our heads. A lot of my work has been teaching other people about that interaction. We can all observe it in everyday life, if we look for it. It’s not mystical or mysterious. It’s evident in the way our expectations determine and limit what we can perceive. To me this is the realm of practical magic, and it should be a part of medicine.






